What is Meniere’s disease?
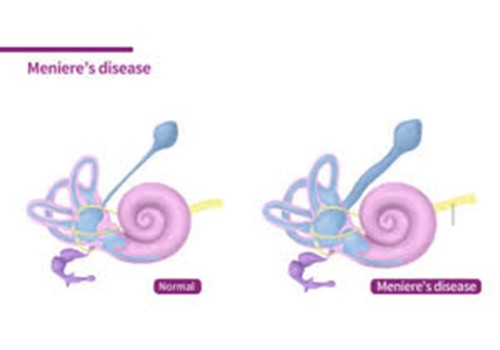
It is idiopathic meaning there is no specific known cause. It is a form of endolymphatic hydrops which occurs due to an increase in endolymphatic fluid in the inner ear which causing a recurring set of symptoms. It can occur at any age but most common between 40-60 years old.
At present the exact cause is unknown but a few theories have been looked into which include circulation issues, viral infection, autoimmune response, migraine and a possible genetic link. Symptoms typically present as an ‘attack’ or episode. Some triggers may include stress, overwork, fatigue, emotional distress, illness, pressure changes, certain foods or too much sodium/salt.
Symptoms:
These can vary throughout the progression of the disease. Typical symptoms of an attack include spontaneous vertigo, fluctuating hearing loss and ear fullness/tinnitus lasting between 20 minutes to 12 hours. Attacks can occur days, weeks, months or even years apart. Symptoms can vary before, during and after an attack. Changes to hearing typically only occur in one ear.
You may experience an ‘aura’ before an attack which is a specific set of symptoms that may warn you of an oncoming attack and allow you to make yourself safe before these occur. The variability in symptoms can make is a challenging disease to study.
Diagnosis:
Monitoring your hearing during or after attacks is helpful as well as getting regular audiological testing to monitor any changes in hearing.
The Bárány Society established the following diagnostic criteria for Ménière’s disease. The following criteria must be met for the diagnosis of Ménière’s disease:
- Two or more spontaneous episodes of vertigo, each lasting 20 minutes to 12 hours.
- Audiometrically documented low- to medium frequency sensorineural hearing loss in one ear, defining the affected ear on at least one occasion before, during, or after one of the episodes of vertigo.
- Fluctuating aural symptoms (hearing loss, tinnitus or fullness) in the affected ear.
- Not better accounted for by another vestibular diagnosis.
Medical treatment:
There is currently no cure to eliminate Meniere’s disease however medical treatments can help to manage the symptoms. Current medical treatments look to reduce the severity, frequency and number of attacks.
Medication:
You may wish to speak to your GP or Ear, Nose and Throat consultant about medication which can help to manage some of the symptoms associated with Menieres disease both during and between attacks.
- Anti-vertigo medications
- Diuretics
- Corticosteroids

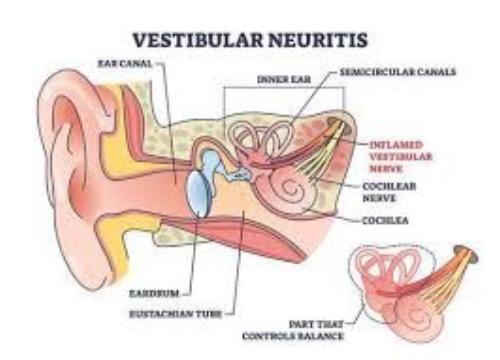
Physiotherapy as treatment:
Vestibular Rehabilitation is indicated for people who’s condition is stable and well managed to help with feeling of dizziness and imbalance. Vestibular rehabilitation is a customisable and individualised approach to managing the above symptoms which occur between the attacks or episodes.
Vestibular rehabiliatation cannot change Menieres disease however it can help with the symptoms that can occur between attacks such as the feeling of imbalance, dizziness, unsteadiness and some visual difficulties.
Conservative treatment:
Life style changes-
- Moderate exercise
- Reducing stress
- Low sodium diet (1500-2300mg/day)
- Reducing caffine, alcohol and tabacco useage
Surgery:
In some case your doctor may consider surgery as an appropriate option to manage symptoms in severe cases.
References:
Vestibular Disorders Association. (2025a). Ménière’s Disease. [online] Available at: https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/menieres-disease/?gad_source=1&gclid=CjwKCAiAiaC-BhBEEiwAjY99qGoQEjx77HgxUOaw43vAykPvjIAEwWpLd2zRN2J-rjLATsVz2km_TRoCS9oQAvD_BwE [Accessed 7 Mar. 2025].
Mohseni-Dargah M, Falahati Z, Pastras C, Khajeh K, Mukherjee P, Razmjou A, Stefani S, Asadnia M. Meniere’s disease: Pathogenesis, treatments, and emerging approaches for an idiopathic bioenvironmental disorder. Environ Res. 2023 Dec 1;238(Pt 1):116972. doi: 10.1016/j.envres.2023.116972. Epub 2023 Aug 28. PMID: 37648189.